Research Leads to $4.4M From NIH to Use Endolysins as Tools to Eradicate Pneumococcal Biofilms and Development of Protective Immunity
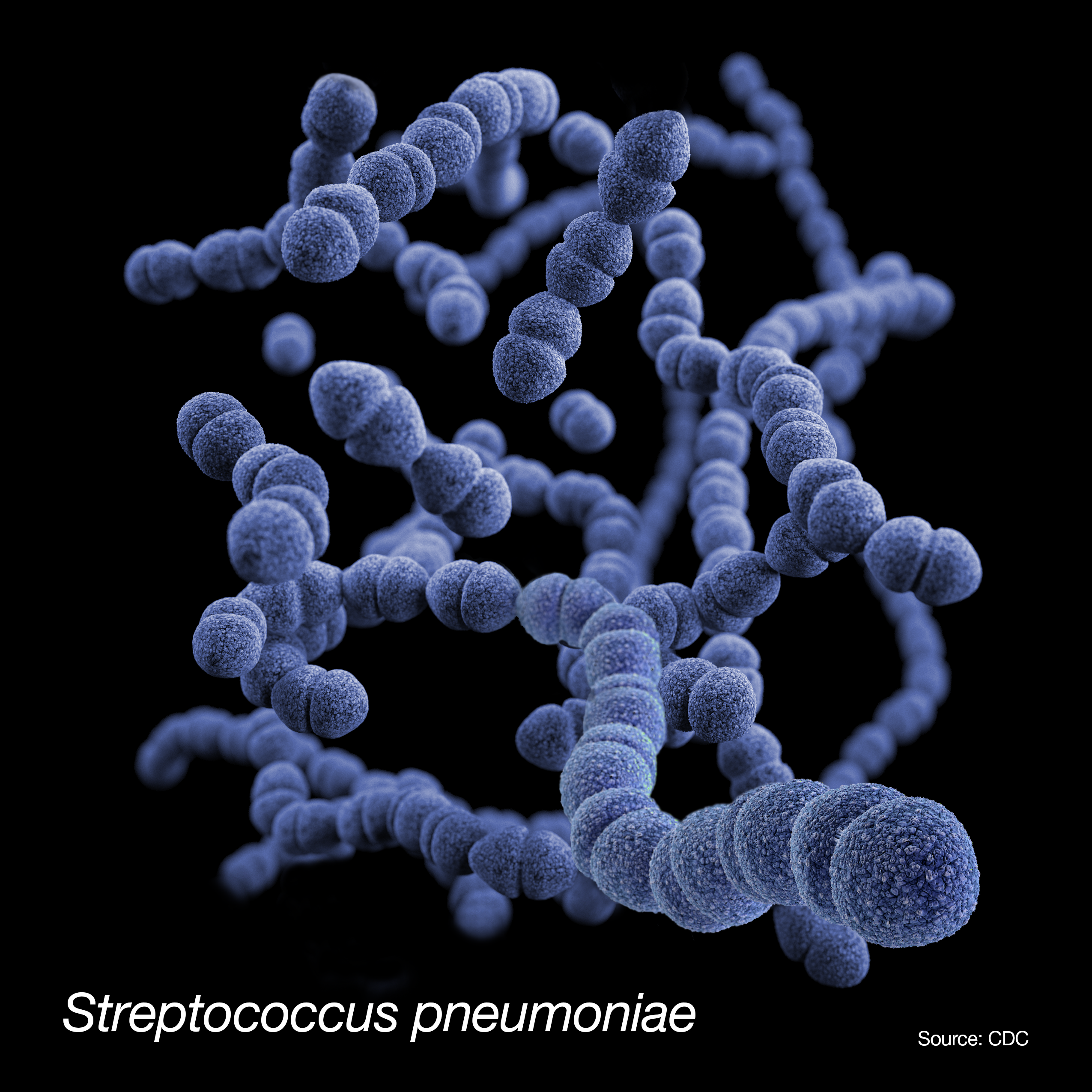
Daniel Nelson, Professor, Department of Veterinary Medicine, University of Maryland, College Park and IBBR Fellow and Norberto Gonzalez-Juarbe, Associate Professor at the J. Craig Venter Institute (JCVI) were recently awarded a $4.4M grant from the NIH entitled, “Endolysins as tools to eradicate pneumococcal biofilms and development of protective immunity.” This grant proposes to develop both a novel therapeutic and vaccine approach to address Streptococcus pneumoniae, the leading cause of bacterial community-acquired pneumonia worldwide.
According to the World Health Organization, pneumococcal infection causes more than 1.6 million deaths annually, with children and the elderly being the most vulnerable demographics. Although very effective against invasive illness, pneumococcal vaccinations are sometimes unavailable in many developing countries. Additionally, just a few of the most prevalent pneumococcal serotypes are targeted by these vaccinations and given that there are over 100 different pneumococcal serotypes, the emergence of disease caused by non-vaccine serotypes is a cause of serious concern.
The development of antimicrobial resistance and the international spread of resistant organisms are factors in the escalating pneumococcal disease crisis. The usage of endolysins is a new strategy being developed to combat the problem of rising antimicrobial resistance. Endolysins are enzymes that can degrade the bacterial cell wall upon contact, killing the bacteria, and represent an alternative to traditional vaccines and antibiotics. Furthermore, because these enzymes function in a species-specific manner, they can only affect pathogenic bacteria while sparing "good" bacteria.
Nelson and Gonzalez-Juarbe have two goals with the use of the grant. First, endolysins will be directly evaluated for their ability to treat active pneumococcal infection. Next, the researchers will use endolysins to cause necroptosis, a form of cell death that initiates the development of protective immunity against colonizing bacteria.
“The use of an endolysin to induce localized necroptosis via bacterial lysis should have a significant impact on development of serotype-independent protective immunity against colonizing bacteria,” said Gonzalez-Juarbe.
Pneumococcal antigens will be released as a result of endolysin-induced bacterial lysis, and when combined with localized necroptosis activity, they are anticipated to aid in the development of an effective immune response to future pneumococcal exposure. In this way, endolysin therapy would provide long-lasting, serotype-independent immunity.
“We have spent many years doing basic research to engineer and optimize the perfect pneumococcal endolysin. Now we are finally ready to move forward with the infection and efficacy studies supported by this award,” said Nelson.
